Guest contribution:
 Article series on the subject of state-of-the-art mycology in dermatology,
Article series on the subject of state-of-the-art mycology in dermatology,
6th article
by Prof Hans-Jürgen Tietz, Director of the Institute of Fungal Diseases in Berlin, Germany
One hot-button word is still going round: Mutations. However, we are not talking of viruses. Also fungi develop in an evolutionary process. These may not be as flexible as most viruses and bacteria from a genetic perspective, but they are often much smarter. This is because their strategy is almost always based on an arrangement with the immune system.
A good example would be chronic vaginal mycosis caused by C. albicans. The affected women are virtually never ill despite the infection, since the pathogen stimulates the immune protection. Basically, many fungal infections are not the disease of the ill as we have learnt, but that of the young and healthy. Onychomycoses in children prove it. The other side of the coin, however, is that many fungal pathogens may stimulate the immune system, but do not allow immunity against themselves. They undermine the defence by a kind of cease-fire which is advantageous for both sides. The pride of evolution − Charles Darwin would be thrilled.
One disadvantage of this symbiosis is that there are no vaccines providing protection from mycoses. If no immunity can be achieved the natural way, a vaccine won’t achieve it either. The ringworm in cattle is an exception.
Fungal pathogens can also mutate. A current and problematic example is the resistance of some species to terbinafine. This is a shock to mycology, since terbinafine was considered as the most effective substance to fight dermatophytes. The resistance to terbinafine applies to classics, i.e. T. rubrum, as well as subspecies, such as T. mentagrophytes of types VII and VIII, which first came here from Thailand and India.
In the case of T. rubrum, there are punctual mutations in the squalene epoxidase gene, which is the sole target of terbinafine [1, 2]. Whether the new variants are acquired or constitute a primary “God-given” resistance still remains unknown. One way or the other, Darwin would have been at least delighted by the new diversity in species in mycology, since this is the best proof that species do not only extinct, but new species are still appearing today.
From a diagnostic view, none of the two types poses a problem. The EUROIMMUN microarray allows fast and reliable identification of the two as T. mentagrophytes. Both pathogens have a different phenotype with respect to both clinic and culture. Whoever witnessed T. mentagrophytes type VII once will never forget it. Its presentation on the skin is dramatic, possibly due to its young evolutionary age and immunological foreignness. Its culture is equally impressive. However, it is only slowly growing and the subcultures rapidly lose their beautiful burgundy pigmentation. Colonies of type VIII are rather inconspicuous. An exact nomenclature for the two pathogens is still missing.
Type VII is mainly sexually transmitted, which is why it was the first dermatophyte to be classed as STD. This has been an absolute novelty. The exact genetic differentiation of both types in the EUROIMMUN microarray is also imminent only after a short time.
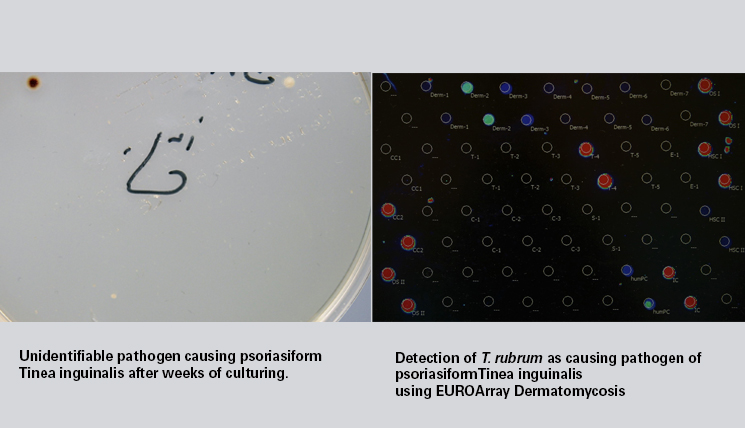
Today’s patient is a good example of the great progresses genetic diagnostics is making today. The strong clinic evokes the name “Thailand fungus”. After weeks, the culture only showed a small fungus, without any chance for conventional identification (Titel image: Detection of the pathogen causing psoriasiform Tinea inguinalis applying conventional culture and EUROArray Dermatomycosis: T. rubrum). The PCR helped: It was T. rubrum, which prove to be resistant to the previous therapy using terbinafine. Moreover, the terbinafine generic possibly also caused the psoriasiform overreaction of the skin, in alliance with the pathogen. Dermatophytes can be a provocation factor of psoriasis, and also for hyperreactive dermatophytids. It’s only with treatment with itraconazole and ciclopirox that this impressive mycosis finally heals. Conclusion: It’s not quiet at all at the mycological front. The suspense continues.
Yours, Hans-Jürgen Tietz
References
[1] Rudramurthy SM, et al. Antimicrob Agents Chemother 62: e02522-17 (2018) [2] Burmester A, et al. Medical Mycology Case Reports 26: 23-24 (2019)
The articles under the rubric “Guest contribution” only reflect the views of the respective authors. Responsibility for the legality and content of the articles lies solely with the authors. EUROIMMUN does not assume liability for the completeness, accuracy and currentness of the information provided.