Polycystic ovary syndrome (PCOS) is a disorder of the hormone metabolism, which affects around 10% of women in child-bearing age and one of the most common causes of childlessness.
PCOS is often associated with further metabolic disorders and they may reinforce each other. Many women suffering from PCOS are overweight, have an increased risk of developing type II diabetes mellitus or cardiovascular diseases and are more likely to have mild hypothyroidism.
Since PCOS symptoms represent a severe psychological burden for many patients, the disorder is also often associated with depression and anxiety.
PCOS characteristics
The original name of the disorder “Polycystic ovarian syndrome” wrongly leads to the idea that the disease is accompanied by formation of many cysts in the ovaries. However, ultrasound images of affected women only show a higher number of follicles, which are neither cysts, nor tumours. Nonetheless, the patients do not ovulate.
The third characteristic of the syndrome is a hormonal imbalance, i.e. hyperandrogenaemia, that is, an increased production of androgens. Androgens, such as testosterone and their precursors, are sex hormones with virilising (masculinising) effect. In women, they are mainly formed in the ovaries and the adrenal cortex.
The increase in the androgen concentration leads to an imbalance of the estrogen metabolism, since a share of the excess androgens is converted into estrogens in the fatty tissue. In the pituitary gland, the increased estrogen level causes an increase in the luteinising hormone (LH), which results in an imbalance of LH to the follicle-stimulating hormone (FSH). One important task of LH is to mediate ovulation, while FSH is responsible for maturation of the ovulation. If there is too little FSH for the amount of LH, the eggs cannot become mature and accumulate in the ovaries. This leads to irregular and seldom or completely absent menstruation.
Moreover, the imbalance of LH to FSH leads to an increased formation of androgens in the ovaries. In this ways, the agents of the hormonal metabolism reinforce each other and hence also the symptoms of PCOS. The visible consequences of increased androgen concentrations in women are acne, alopecia, increased hair growth on the upper lip and chin, chest, abdomen and back, arms and legs (hirsutism). Besides the evaluation of the visible signs of androgenisation, the detection of increased androgen concentrations in blood plays a central role in the diagnostics of PCOS.
PCOS diagnostics
The following applies to PCOS diagnostics: If other diseases can be excluded as the cause of the symptoms, the fulfilment of two of the three typical PCOS characteristics (the so-called Rotterdam criteria): 1. Polycystic ovary, 2. Menstrual disorders, 3. Clinical and/or biochemical signs of hyperandrogenism allow to make a diagnosis.
Androgens and free androgen index
According to the international diagnostic guidelines for PCOS, total testosterone and/or free, bioavailable testosterone as well as measurement of the so-called free androgen index (FAI) which indicates the concentration ratio between total testosterone and sex hormone binding globulin (SHBG). SHBG is a protein produced by the liver, which binds, stored and transports the male sex hormones testosterone and dihydrotesterosterone and the female sex hormones from the group of estrogens, inactiving them for the binding time. A lower SHBG concentration thus leads to a higher concentration of active testosterone. If the concentration of free testosterone is within the normal range and thus does not indicate PCOS, the levels of the testosterone precursors androstenedione and dihydroepiandosterone (DHEA), respectively its metabolite DHEA sulphate (DHEA-S), can be determined in order to detect hyperandrogenaemia.
DHEA is the most important androgen of the adrenal cortex. Since DHEA-S is less dependent on the diurnal or cyclic deviations than DHEA, the determination of the DHEA-S level is often the preferred diagnostic choice. Clearly increased DHEA-S levels indicate an organic cause of the hormonal imbalance in the adrenal cortex. In this case, an enzyme defect (e.g. 21-hydroxylase deficiency leading to accumulation of 17-OH-progesterone and androgen excess, also known as congenital adrenal hyperplasia, CAH) or a tumour must be excluded.
Luteinising hormone and follicle-stimulating hormone
Besides the androgen concentrations, the LH level can be determined and compared to the FSH concentration. Due to the imbalance of the hormone metabolism which is reinforcing itself, the value in PCOS patients is also often increased.
Anti-Mullerian hormone
The determination of the anti-Mullerian hormone (AMH) concentration also becomes more and more important with suspected cases of PCOS, especially in women over 35 years in whom polycystic ovaries are less often detected by ultrasound. Due to increased secretion of AMH in the follicles, the level in PCOS patients is twice as high or even three times as high as in healthy women of the same age.
Serological investigations thus pursue different goals:
- On the one hand, other diseases of the pituitary gland, the adrenal gland, the ovaries and thyroid, which may lead to similar symptoms, must be excluded; among other things, this requires determination of 17-OH-progesterone to exclude AGS and of TSH to check the function of the thyroid.
- On the other hand, the concentration of male and female sex hormones is measured in order to exclude possible tumours of the ovaries and also to confirm the presence of a PCOS.
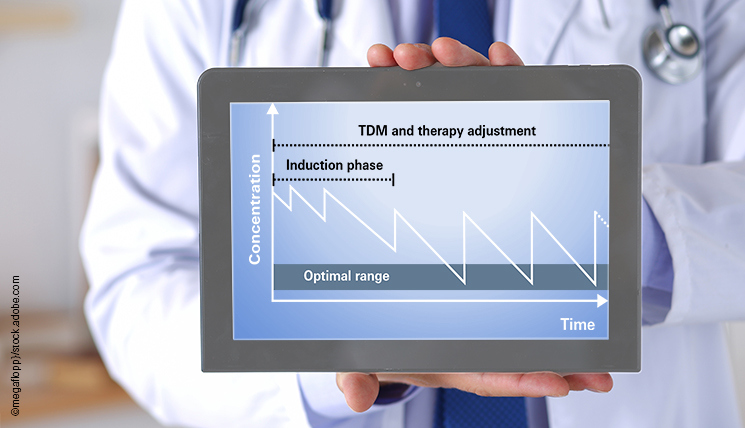
ELISA for determination of hormone levels in blood
EUROIMMUN offers an extensive range of ELISAs for the determination of different hormones which may be related to PCOS. A special validation for automated processing on the EUROIMMUN Analyzers has been performed for all test systems.
*available soon **with sales restrictions