Diagnosis of acute Lyme neuroborreliosis
Since 2005, the chemotactic cytokine (chemokine) CXCL13 has been considered a potential biomarker for acute Lyme neuroborreliosis [1, 2]. Lyme neuroborreliosis is the neurological manifestation of tick-borne Lyme disease which is caused by the spirochete Borrelia burgdorferi sensu lato and frequently occurs in the northern hemisphere. Symptomes of Lyme neuroborreliosis include inflammation of the central nervous system and peripheral nerves and nerve roots (meningoradiculitis, often with paresis of cerebral nerves).
According to European guidelines, an intrathecal synthsis of specific anti-Borrelia antibodies has to be demonstrated for a definite diagnosis of acute Lyme neuroborreliosis, together with characteristic neurological symptoms and cerebrospinal fluid (CSF) pleocytosis [3]. However, an elevated anti-Borrelia antibody index cannot be detected in up to 20% of early Lyme neuroborreliosis cases [4, 5]. In contrast, different studies reported increased CXCL13 concentrations in CSF of patients with acute Lyme neuroborreliosis already in initial phases of disease, even in cases without detectable intrathecal antibody synthesis [1, 5, 6].
The chemokine CXCL13 – a new biomarker
CXCL13 is secreted into CSF by monocytes and dendritic cells which interact with lipoproteins of the bacterial plasma membrane via the toll-like receptor 2. The chemokine attracts B cells which migrate into the CSF. After differentiation into plasma cells, they produce specific anti-Borrelia antibodies. This casual chain of events requires an increase of the CXCL13 level in CSF prior to activation of intrathecal antibody synthesis. Therefore, the chemokine CXCL13 may be sensitively detected already in early stages of Lyme neuroborreliosis [6, 8].
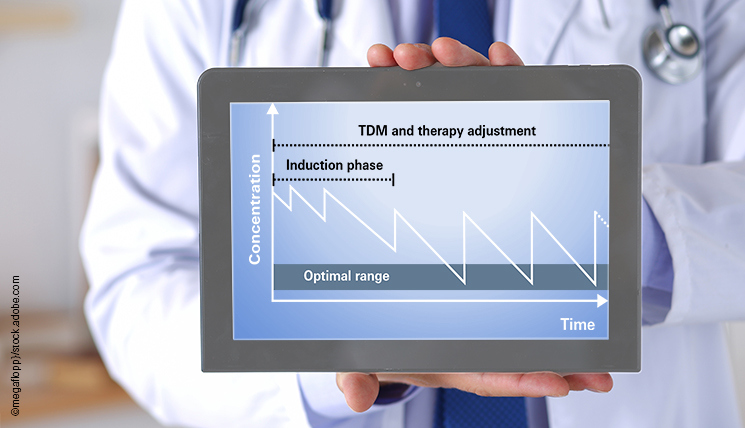
In Lyme neuroborreliosis patients under antibiotic therapy, CXCL13 rapidly decreased in the context of another study. The anti-Borrelia antibody index did not show any corresponding response [9]. Specific anti-Borrelia antibodies can persist in CSF and serum for years despite successful therapy. Thus, determination of CXCL13 concentration, but not the antibody index, may be suited to Lyme neuroborreliosis therapy monitoring [10]. A new commercial CXCL13 ELISA can be applied for qualitative and quantitative detection of the chemokine CXCL13 in CSF. It is registered and labeled with the European CE mark.
Further clinical evidence and the characteristic symptoms of acute Lyme neuroborreliosis remain crucial for a definite diagnosis since CXCL13 levels may also be elevated in other inflammatory infections of the central nervous system (e.g. CNS lymphoma, HIV meningitis, streptococcus infection, multiple sclerosis).
[1] Rupprecht et al., 2005 Neurology [2] Narayan et al., 2005 Ann Neurol [3] Mygland et al., 2010 Eur J Neurol [4] Borde et al., 2012 BMC Inf Dis [5] Schmidt et al., 2011 Neurology [6] Rupprecht et al., 2006 Nervenarzt [7] Rupprecht et al., 2009 J Neuroinflam [8] Rupprecht et al., 2008 Mol Med [9] Senel et al., 2010 J Neurol Neurosurg Psychiatry [10] Rupprecht et al., 2014 Nervenarzt