The sex hormones in the human body work together like a complex clockwork. They control not only the development of the female and male sexual characteristics such as the vagina, ovaries and breasts or the penis and testicles, respectively, but also their sexual and reproductive functions. Fluctuations in the balance of sex hormones are normal: Some hormone concentrations vary depending on the time of day or decrease permanently as part of the ageing process. And the female cycle, a prerequisite for human reproduction, would not be possible without the regular increase and decrease of sex-hormone levels. However, aside from these normal fluctuations, sex hormones can also get out of sync, which can cause serious issues.
Function of the sex hormones
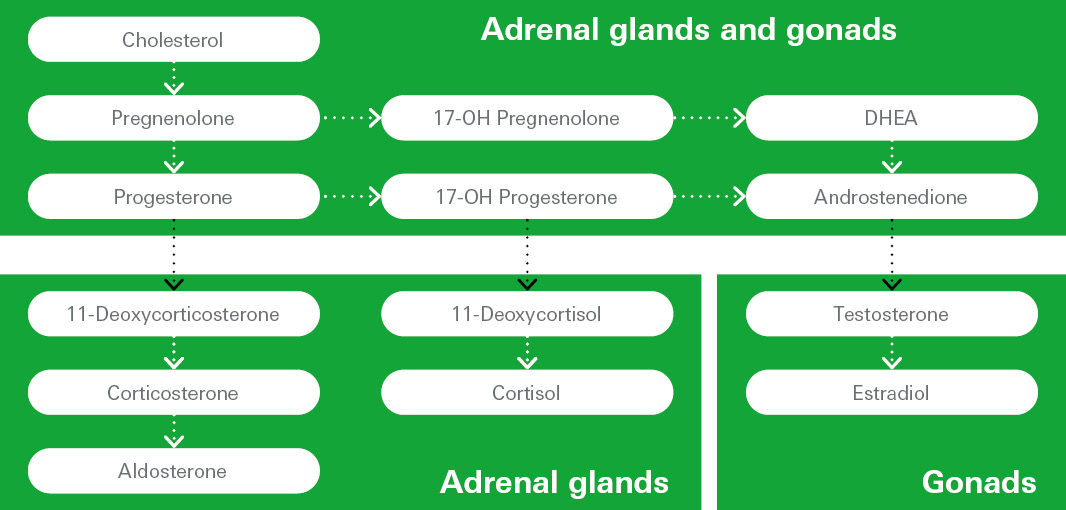
The most important male sex hormone, or androgen, is testosterone – a steroid hormone produced from cholesterol via several intermediate steps (see figure 1). In men, this occurs primarily in the testes. Testosterone not only controls the development of male sexual characteristics during puberty and influences sexual behaviour. It is also essential for maintaining healthy bones, stimulating protein biosynthesis and contributing to the building of muscle mass. It also fulfils the latter functions in the female body, where it is produced in the ovaries – but in much smaller quantities than in men. Around 2% of total testosterone is bioavailable and circulates in the blood of all sexes – either in its free form or bound to the protein albumin. However, the majority of the hormone is inactive due to its high affinity for sex hormone-binding globulin (SHBG).
The direct precursor in testosterone production is the androgen androstenedione, which fluctuates throughout the day. Like testosterone, it is produced in the gonads of both men and women and plays an important role in the production of the different estrogens, the female sex hormones.
Together with gestagens, estrogens and especially estradiol play a central role in the female body. Estradiol is mainly produced in the ovaries from the precursor testosterone (see figure 1). It is essential for the differentiation of female sex organs during puberty and regulates the menstrual cycle in fertile age: The main function of estradiol is the stimulation of ovulation, as reflected by the characteristic fluctuations in the concentration throughout the cycle. Moreover, the hormone is critical for bone health (read also our blog article on bone disorders!) and also takes effect in numerous other sites, such as the brain, blood vessels, skin and hair. Estradiol is also present in the male body, with its non-sex-specific effects, and plays a certain role in the testosterone balance and in sexual function.
Progesterone is a gestagen and is produced in the second half of the female menstrual cycle. It contributes to preparing the body for a potential pregnancy and to maintaining it by working with estradiol to build and remodel the lining of the uterus for embryo implantation. If no pregnancy occurs, a drop in the progesterone level leads to menstruation. Progesterone is produced in both the gonads and the adrenal cortex of both the female and male body (see figure 1). There it is transformed either into 17-OH progesterone via different hydroxylases, or to corticosteroids such as cortisol and aldosterone via different interim stages. The specific functions of progesterone in the male body have not yet been clarified.
In contrast to androgens, estrogens and gestagens, the “breastfeeding hormone” prolactin is in fact not a steroid hormone, but a protein. It is, however, strongly associated with the sex hormones and aids the assessment of disorders such as infertility and hypogonadism. 1, 2 Prolactin is synthesised in the anterior pituitary and secreted in large quantities during pregnancy and in the first months after birth. It primarily stimulates milk production in the female breasts and simultaneously inhibits a new pregnancy during the breastfeeding period.
Sex-hormone imbalances
Disturbances in this intricate “clockwork” of sex hormones are relatively common and can cause the following disorders:
- Puberty disorders – such as a significantly earlier or later onset of puberty. 3
- Hypogonadism (hypofunction of the gonads) 4: In men, this is characterised by the feminisation of the body due to low testosterone production; in women, by the absence of the menstrual period (amenorrhea). In both sexes, it impairs sexual function and fertility and increases the risk of osteoporosis.
- Hyperandrogenism (androgen excess): A typical example is polycystic ovary syndrome (PCOS) in women. 5 Due to increased androgen levels in the blood, patients often experience masculinisation and issues with their menstrual cycles. PCOS is one of the most common endocrine disorders in women of fertile age and is often associated with infertility.
- Disorders such as CAH (congenital adrenal hyperplasia) 6: In the case of an enzyme defect in the hydroxylase responsible for the first step of the conversion of progesterone/17-OH progesterone into cortisol, then cortisol deficiency occur will occur. The body’s attempt to compensate it leads to an increased 17-OH progesterone concentration and hyperandrogenism.
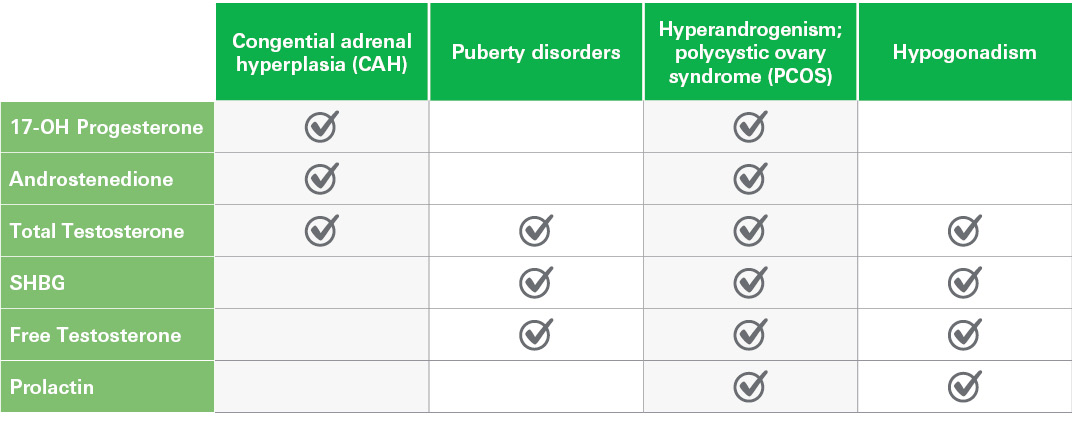
These endocrine disorders typically affect patients both physically and mentally. An unfulfilled desire for children due to reduced fertility is a particular burden for the affected couple. However, the hormonal imbalance at its cause can be treated well, provided that early, targeted and comprehensive diagnostics are carried out. These should include careful evaluation of the clinical picture in combination with laboratory diagnostic tests to determine the levels of the different sex hormones in order to reveal any existing hormonal imbalances (see figure 2).
Assays for the detection of sex-hormone imbalances
Endocrine-related sex-hormone imbalances can be identified reliably and assessed thanks to high-quality diagnostic test systems, such as those from the ever-increasing range of chemiluminescence assays from EUROIMMUN and IDS (see figure 2):
- IDS Free Testosterone
- IDS Total Testosterone
- IDS SHBG
- IDS Androstenedione
- IDS 17-OH Progesterone
- IDS Prolactin
The assays can be processed fully automatically on the same platform – one sample tube is sufficient for several hormone determinations, which makes blood collection less burdensome. Reliable and precise results are available quickly and support healthcare professionals in therapy decisions.
Did we spark your interest? Discover our endocrinology panels and parameters and learn more about diagnostics in this area! If you would like to know more about endocrine disorders, take a look at the other blog articles in this series covering the topics of growth disorders, bone disorders and endocrine hypertension!
References:
1. Fahie-Wilson M, Smith TP. Determination of prolactin: the macroprolactin problem. Best Pract Res Clin Endocrinol Metab 27(5):725 – 742 (2013).
2. David G, et al. Evaluation of the analytic performance and macroprolactin sensitivity of a new prolactin immunoassay. Ann Endocrinol (Paris) 86(2): 101677 (2025).
3. Latronico AC, et al. Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol 4(3): 265 – 274 (2016).
4. Khera M, et al. Adult-Onset Hypogonadism. Mayo Clin Proc 91(7):908 – 926 (2016).
5. Joham AE, et al. Polycystic ovary syndrome. Lancet Diabetes Endocrinol 10(9):668 – 680 (2022).
6. Speiser PW, et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 95(9):4133 – 4160 (2010).

