This is about two diseases with very similar symptoms, but completely different causes: chikungunya virus infection and rheumatoid arthritis.
The chikungunya virus (CHIKV) is transmitted to humans by mosquito bites, particularly from yellow fever mosquito (Aedes aegypti) and the Asian tiger mosquito (Aedes albopictus). These insects may not only transmit CHIKV, but also dengue fever, yellow fever and West Nile viruses. CHIKV was first discovered in at the beginning of the 1950s in Tanzania. Later, cases were reported in Western Africa and in India and South East Asia. In recent years, the mosquitoes and consequently, the virus have spread alarmingly fast, for example in the Caribbean and South America.
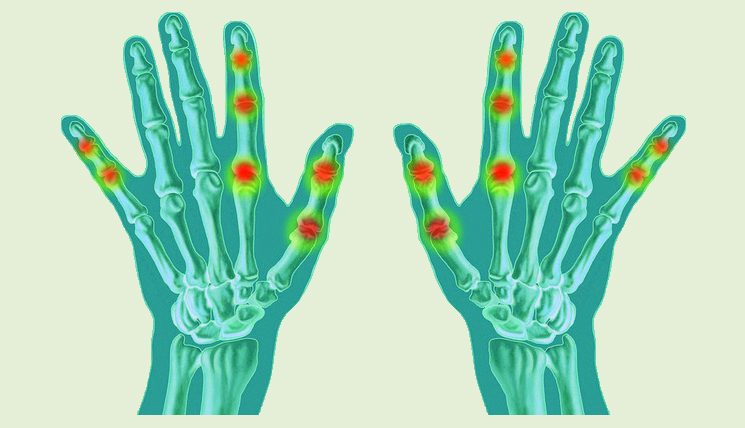
After an incubation period of 3 to 7 days, CHIKV infections usually lead to an abrupt fever outbreak, severe head ache and swollen joints which are extremely sensitive to touch. These symptoms frequently occur together with a blotchy rash (exanthema) or generalised redness of the skin. In the majority of patients, the symptoms abate without therapy. Complications or permanent damage are rather rare. Up to 10% of patients, however, suffer for months or in rare cases even years from painful joint inflammation which may severely impair their mobility. Since affected persons can hardly stand up straight, the disease was named chikungunya, which means “crookedly walking person” in the language of the Makonde people, an ethnic group from East Africa. This so-called chikungunya-associated arthritis occurs symmetrically in the joints of the left and right halves of the body, very much like in rheumatoid arthritis.
In contrast to the tropical disease however, rheumatoid arthritis (RA) is an autoimmune disease where inflammation and damage of the joints is caused by an immune response against the body’s own structures. RA is diagnosed using established classification criteria of the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) which take into account the following factors: number and size of the affected joints, duration of the inflammation, serology (determination of rheumatoid factors and autoantibodies against cyclic citrullinated peptides (ACPA) in serum), and general inflammatory markers. If a defined number of these criteria applies in a patient and no other possible cause for the complaints is indicated, the diagnosis RA is considered certain.
However, as shown by a study published in May in the USA, the criteria may also be sufficiently met by chikungunya-associated arthritis. Miner et al. showed that 8 out of 10 patients with joint inflammations who had a known CHIKV infection would have been classified as (seronegative) RA patients according to the ACR/EULAR criteria (2010) if there had not been any information on their visit to Haiti, even though no RA-specific autoantibodies or rheumatoid factors could be detected in the collected blood samples.
What may first look like a (seronegative) RA could therefore in some cases actually be an infection with CHIKV.
Further symptoms, as well as clarification of recent visits to risk areas and additional blood tests can confirm the diagnosis. Following the sixth day after onset of first symptoms, usually specific IgM, IgG against the virus are detectable in serum using serological tests (ELISA, indirect immunofluorescence). Those who have recovered from an infection are presumed to have life-long immunity against CHIKV.